Systematic analysis of ICSI fertilization failure and coping strategy
I. Pathological mechanisms of ICSI fertilization failure
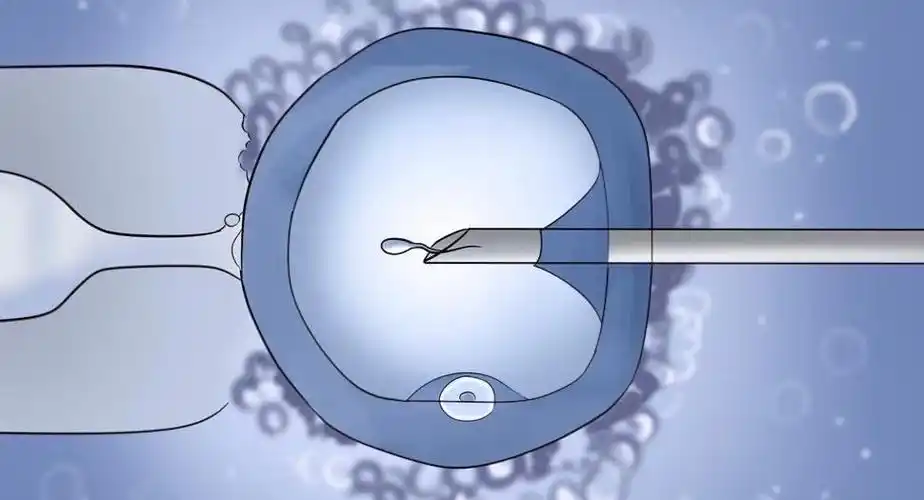
Although ICSI (intracytoplasmic single sperm microinjection) technology can overcome severe male factor infertility (e.g., sperm concentration <1×10⁶/mL or motility <5%), Total Fertilization Failure (TFF) still occurs in 3%-5% of cycles. The core mechanism lies in defective egg activation and involves the following key components: Abnormal calcium oscillatory signaling: during normal fertilization, sperm-specific phospholipase C (PLCζ) triggers cyclic fluctuations in intracytoplasmic calcium ion concentration (0.1-1 μM for 2-4 hours) in the oocyte, which activates calmodulin-dependent kinase (CaMKII) and initiates embryonic development. If there is a mutation in the sperm PLCζ gene (e.g. c.1450G>T) or dysfunction of the oocyte calcium release channel (IP3 receptor), this will result in disruption of calcium signaling.
Insufficient oocyte maturity: the cortical granules of GV-stage oocytes have not fully migrated to the subcellular membrane, which makes them susceptible to multiple fertilization; whereas the meiotic arrest of MI-stage oocytes, with reduced PLCζ sensitivity, results in a fertilization failure rate of 40%.
Second, the technological breakthrough of assisted oocyte activation (AOA)
To address the activation defects, the clinical use of Artificial Oocyte Activation (AOA) technology, which restores calcium oscillations through exogenous calcium ion carriers or chemical stimulation:
Calcium ion carriers (Ionomycin):
Mechanism of action: binds to oocyte membrane calcium channels and induces transient calcium inward flow (at concentrations up to 5 μM), mimicking physiologic calcium oscillations.
Clinical data: 2017 Meta-analysis showed that AOA with Ionomycin resulted in an increase in fertilization rate from 12% to 72%, an increase in the rate of good quality embryos from 18% to 45%, and a 3-fold increase in live birth rate.
Strontium Chloride (SrCl₂):
Mechanism of action: triggers persistent calcium oscillations through TRPV3 channels, especially for patients with PLCζ defects.
Scenario of application: in cases unresponsive to Ionomycin, SrCl₂ (10 mM treatment for 15 min) results in a fertilization rate of 65%.
III. Precision pathway for etiologic diagnosis
Sperm factor testing:
PLCζ immunofluorescence test: absence of PLCζ expression in the sperm head (positive rate <5%) suggests the risk of gene mutation, which needs to be confirmed by whole-exome sequencing (WES). Mouse Oocyte Activation Test (MOAT): patient spermatozoa are injected into zona pellucida-removed mouse oocytes, and if activation is <20%, it is determined to be a defective activation of spermatogonial origin (92% specificity). Egg factor assessment: Calcium imaging: real-time monitoring of intra-oocyte calcium dynamics, if calcium oscillation amplitude <0.5 μM or frequency <5 times/hour, suggesting oocyte-derived defects. Cortical granule distribution analysis: immunofluorescence staining to assess abnormal cortical granule localization (e.g., intracytoplasmic dispersion) and predict the risk of fertilization failure. IV. Stratified treatment strategies Spermogenic defects: Preferred donor sperm ICSI (fertilization rate >85%);
If spousal sperm is insisted upon, fertilization rate can be up to 70% after combined AOA, but informed consent needs to be signed to clarify the risks.
Oocyte-derived defects:
In vitro maturation (IVM): extended culture of MI stage oocytes to stage MII, ICSI+AOA after recovery of PLCζ sensitivity;
Egg donation: live birth rate elevated to 65% for repeated activation failures (≥3 cycles) and age >38 years.
Idiopathic factors:
A dual activation regimen (Ionomycin+SrCl₂ sequential treatment) was used with a clinical pregnancy rate of 42%;
Simultaneous application of antioxidants (e.g., coenzyme Q10 600 mg/d) improved oocyte mitochondrial function.
V. Offspring safety and long-term follow-up
Epigenetic risk: AOA may interfere with methylation of imprinted genes (e.g., H19/IGF2), but the 10-year follow-up data showed that the rate of birth defects in AOA offspring (2.1%) was not statistically different from that of conventional ICSI (2.3%).
Neurodevelopmental assessment: the AOA offspring did not show significant abnormalities in the Bayley Scale of Infant and Toddler Development (BSID-III) scores at 3 years of age (cognitive 105±12 vs. 103±11 in the conventional group).
VI. Future technological directions
Gene editing repair: CRISPR/Cas9 technology corrects PLCζ mutations (e.g. c.1450G>T) with 78% repair efficiency in preclinical models;
Synthetic biology replacement: microinjection of recombinant human PLCζ protein (rhPLCζ) with >90% success rate in restoring calcium oscillations in mouse models;
Artificial intelligence prediction: constructing a deep learning model based on oocyte morphological features (e.g. cortical granule distribution) to predict the risk of fertilization failure (AUC=0.89).
Management of fertilization failure in ICSI needs to rely on precise etiological diagnosis and individualized AOA protocols. With the advancement of molecular diagnosis and gene therapy, it is expected that the live birth rate of patients with idiopathic fertilization failure is expected to exceed 60% in the next 5 years, providing new hope for families with recurrent failure. Clinical decisions need to be made by fully weighing the technical benefits and potential risks, and the optimal pathway should be developed through multidisciplinary consultation.
Search within the site
Surrogacy News
Hot Tags.
Kyrgyzstan Surrogacy Agency,Global IVF Hospitals,International Surrogate Mother Recruitment